Favorable Effects of Pregnancy on Disease Activity of Systemic Lupus Erythematosus
INTRODUCTION
The view that systemic lupus erythematosus (SLE) is a disease which commonly compromises pregnancy and disease itself is genrerally accepted. Is it true?
I presented here an SLE patient whose serological markers were getting better in paralleled with the course of her pregnancy.
CASE REPORT
A 31-year-old woman consulted our hospital at Aug. 2004 because she awoke her migratory polyarthralgia. Five years ago, she had been told that her immunoserological data contained any abnormal result(s). However, no treatment has been done.
At first consultation, when she was not yet pregnant, the physical examination showed that there were no obvious butterfly rash, lupus hair, and oral ulcerations. Laboratory data at that time showed positive antinuclear antibodies (ANA) at ×640 (homogeneous/speckled patterns) and positive anti-DNA antibody at a level of 49.8 IU/mL (normal: less than 6.0). Her anti-SS-A/Ro, anti-beta2 glycoprotein I (ΐ2-GPI), and anti-Sm antibodies were all negative. By repeated examinations, a slight leukopenia was found (2,900` 4,000/cmm). Her urinalysis was normal.
A diagnosis of SLE was made. Three months later, when she consulted us for the purpose of followin up, we knew that she got pregnant four weeks ago. This was her second pregnancy.
We decided to stand by without any medical intervention unless any deterioration would occur in her clinical symptoms and/or in laboratory markers, because we considered that her disease activity was rather mild.
|
|
TP |
Alb |
alpha-1 |
alpha-2 |
beta |
gamma |
IgG |
IgA |
IgM |
anti-DNA |
CH50 |
WBC |
CRP |
|
PRE |
8.1 |
4.81 |
0.21 |
0.58 |
0.58 |
1.90 |
2,163 |
351 |
89 |
49.8 |
35 |
3.900 |
0.1 |
|
10W |
7.6 |
4.32 |
0.27 |
0.58 |
0.71 |
1.61 |
1,751 |
287 |
59 |
26.4 |
41 |
5,100 |
0.1 |
|
27W |
6.9 |
3.85 |
0.31 |
0.66 |
0.72 |
1.35 |
1,504 |
257 |
61 |
18.9 |
44 |
6,900 |
0.0 |
|
18M* |
7.7 |
4.43 |
0.21 |
0.66 |
0.73 |
1.67 |
1704 |
326 |
58 |
31.6 |
36 |
4,000 |
0.0 |
|
|
g/dL |
© |
© |
© |
© |
© |
mg/dL |
© |
© |
IU/mL |
U/mL |
/cmm |
mg/dL |
18M*: 18 months after her delivery. with 5 mg daily of prdnisolone
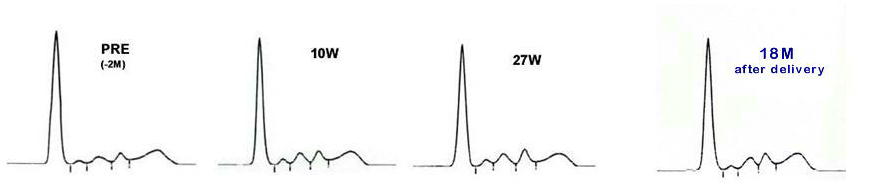
Changes in laboratory data during the pregnancy are shown in the figure and the table.
The serum electrophoretic pattern of just before pregnancy (PRE) showed a hypergammaglobulinemia without an elevation in alpha-2 globulin, which was compatible with the typical figure of SLE. The pattern of her 10 weeks pregnancy (10W) the gammaglobulin decreased and beta globulin increased, as compared with PRE. The pattern of her 27 weeks pregnancy (27W) showed a marked decrease in gamma globulin in contrast with the towering of beta globulin fraction, which might be caused by an increase in transeferrin concentration.
Her anti-DNA antibody titers and serum IgG (IgA) levels decreased in paralleled with the course of the pregnancy. The white blood cell (WBC) returned to normal level.
The migratoroy polyarthralgia which was her only subjective symptom was ameliorated accordingly. Just before delivery (36W), her anti-DNA antibody titer further improved at the level of 11.0 IU/mL. At 39 weeks' pregnancy she gave birth to a healthy female baby whose body weight was 2,800 g.
The serological data at 3 weeks after the delivery, the anti-DNA antibody increased to a level of 18.5 IU/mL, and IgG, IgA, and IgM also increased to the levels of 1,734, 333, and 97 mg/dL, respectively. The administration of daily 5 mg of prednisolone was begun, and 2 years after the delivery, her DNA-antibody titers were stable at the levels of 20-30 IU/mL with a daily 5 mg prednisolone. High dose prednisolone therapy has never been employed. Slight migratory polyarthralgia was still present as her only symptom.
DISCUSSION
The disease activity of this patient improved in paralleled with the "natural" course of her pregnancy. We would like to assure that this was a favorable effect of pregnancy on SLE, because, in spite of no medical intervention was done in the period, the considerable recovery was seen in her anti-DNA antibodies accompanying improvement in serum gamma globulin and IgG levels which are also reliable parameters of the disease activity in autoimmune diseases.
It has been accepted that SLE in pregnancy is associated with unfavorable effects on maternal outcome. Although the clear explanation has not yet been established, in pregnant lupus patients the shift of immune response from TH1 to TH2 may cause an excessive autoantibody production which results in lupus flare. This shift of immune process is considered to be closely related with an increased secretion of estrogen during the pregnancy.
On the other hand, the recent studies indicate that pregnancy in patients with SLE is not a high risk condition for mother (and baby), when careful management of conception is done.
The course of the patient presented here agrees nether with the stereotyped concept that the pregnancy is at risk in SLE, nor with the recently accepted one that the pregnancy is rather safe. The feature of this patient indicates that, at least in some cases of SLE, the disease activity can be ameliorated by their pregnancy. This may be the third and new conception, Further accumulation of persistent case reports and much more studies are needed to clarify the relationship of pregnancy and disease activity of lupus.
REFERENCES
1. Viegas OA, Boey ML. Pregnancy in patients with systemic lupus erythematosus. Singapore Med J 1992.;33:70-3.
2. Ostensen M. Sex hormones and pregnancy in rheumatoid arthritis and systemic lupus erythematosus. Ann NY Acad Sci 1999;876:131-43.
3. Cervera R, Font J, Carmona F, Balasch J. Pregnancy outcome in systemic lupus erythematosus: good new for new millenium. Autoimmun Rev 2002; 1: 354-9.
Takatoshi INOUE (Feb 07)