Sjogren Syndrome
Eight Years' Observation of Two Cases
CASE 1: 47-year-old woman
DIAGNOSIS: Primary Sjogren('s) syndrome (SS)
Table 1.
|
g/dL |
TP |
Alb |
alpha-1 |
alpha-2 |
beta |
gamma |
|
97/06/17 |
7.9 |
4.2 |
0.20 |
0.70 |
0.81 |
1.94 |
|
98/08/19 |
6.5 |
4.0 |
0.16 |
0.58 |
0.68 |
1.04 |
|
01/11/15 |
7.4 |
4.5 |
0.19 |
0.62 |
0.75 |
1.32 |
|
05/12/14 |
7.5 |
4.13 |
0.21 |
0.70 |
0.77 |
1.69 |
Table 2.
|
mg/dL |
CRP |
alpha-1AT |
HP |
IgG |
IgA |
IgM |
A-SSA-Ab |
|
97/06/17 |
0.9 |
166 |
147 |
2090 |
370 |
147 |
256 X |
|
98/08/19 |
0.1 |
131 |
96 |
1270 |
260 |
58 |
64 X |
|
01/11/15 |
not available |
¢« |
¢« |
¢« |
¢« |
¢« |
¢« |
|
05/12/14 |
0.0 |
|
|
1813 |
353 |
91 |
(+) |
CLINICAL COURSE:
She was found as having IgM rheumatoid factor by a health check. She had a few yeas' history of slight sensation of dry eyes and dry mouth.
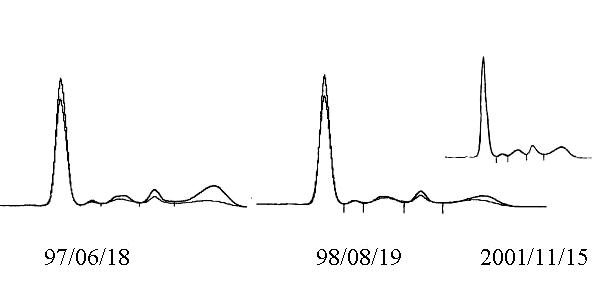
At the first consultation (Jun.06), her IgM rheumatoid factor and anti-SSA(Ro) antibody were both positive. No extra glandular manifestation was found, and a diagnosis of primary Sjogren syndrome (SS) was made. The serum concentration of gamma globulin and of all three classes of immunoglobulin were markedly elevated.
Her Schirmer test was positive (5 mm and 4 mm). The histopathology of her minor salivary glands of the lip showed a focal lymphoid cell infiltrate consistent with class II of Chisholm and Masson index (Class II; one focus of lymphocytic infiltration per 4 cmm of the tissue).
Daily 15 mg of prednisolone was started at Jun.06 and the dose was gradually decreased after one year's therapy. Daily 5 mg maintenance therapy has been continued until now (Mar. 2007).
During the first year of the treatment, while her subjective dry eyes and dry mouth were only slightly ameliorated, polyclonal hypergammaglobulinemia markedly improved to normal levels (Figure and Tables). The Schirmer test slightly improved (right from 5 to 6, left 4 to 10 mm). The histology of incisional minor salivary glands showed a decrease in the infiltrated lymphocytic cell population.
In spite of the maintenance therapy with daily 5 mg prednisolone, her serum immunoglobulin levels gradually increased nearly to the pretreatment level. The patient have never recognized any increase in her subjective sicca symptoms (Feb/07),
CASE 2: 57-year-old woman
DIAGNOSIS: primary SS
http://uda.ehoh.net/PROTHOME.HTML
Table
|
g/dL |
TP |
Alb |
alpha-1 |
alpha-2 |
beta |
gamma |
|
98/08/05 |
8.3 |
4.60 |
0.14 |
0.59 |
0.61 |
2.38 |
|
99/07/22 |
6.4 |
4.10 |
0.12 |
0.50 |
0.52 |
1.22 |
|
05/08/17 |
7.1 |
4.47 |
0.15 |
0.58 |
0.63 |
1.27 |
Other data are not available.
CLINICAL COURSE:
Her anti-SSA(Ro) antibody was positive. The Schirmer test was negative (15 mm and 13 mm). .Histopathology of her minor salivary glands revealed focal periductal lymphocytic infiltration.
After one year's administration of daily 15 mg prednisolone, the hypergammaglobulinemia was improved to normal level.
Daily 5 mg of prednisolone therapy has been continued until now (Feb. 07), without any relapse in her hypergammaglobulinemia.
COMMENTS:
SS is regarded as one of the autoimmune diseases, because several autoantibodies, including rheumatoid factors, anti-SSA(Ro) and anti-SSB(La) antibodies, are present in the patients' serum. However, the use of corticosteroid for this disease has not been authorized except for to the cases with extra glandular or severe systemic manifestations, mainly because that corticosteroid can't prevent the progression of immunopathologic process, and can't ameliorate the subjective dry sensations. In addition, even as a small dose, the side effects of corticosteroid must not be ignored.
The hypergammagolbulinemia of SS is usually very marked, and the cause is not yet unclear. But, it is reasonable to consider that the polyclonal hypergammaglobulinemia in SS must be associated to lymphocyte proliferation in the lachrymal and salivary glands and other affected lymphatic tissues.
Introduction therapy for SS with daily 15 mg of prednisolone was undoubtfully effective to improving clinical symptoms and gamma globulin level, meanwhile the effect of long term maintenance therapy with 5 mg daily of prednisolone was not confirmed. But we would expect that more sophisticated way in corticosteroid use must bring us favourable effects in preventng the disease progression.
REFERENCE
Fox RI, Howell FV, Bone RC, Michelson P. Primary Sjogren syndrome: clinical and immunopathologic features. Semin Arthritis Rheum 1984;14:77-105.