Coexistence of Polyclonal and Monoclonal Hypergammaglobulinemia
INTRODUCTION
A case whose serum protein electrophoretic pattern showed a bizarre figure is presented. The coexistence of monoclonal- with polyclonal-hypergammaglobulinemia in a person as found in this patient is very rare incident. The interpretation of the electrophoretic pattern and the cause(s) of this event are discussed.
CASE PRESENTATION
PATIENT: 65-year-old woman
CHIEF COMPLAINT: Intractable gingival bleeding after a dental operation
PRESENT ILLNESS:
In November '08, after an extraction of her teeth, her gingival bleeding was intractable. Until the episode, she had been subjectively almost well except for slight dry sensation of her mouth and eyes.
Physical examination revealed moderate anemia in her palpebral conjunctiva, and slight edema in her lower legs. Her chest and abdomen was physically within normal limits (WNL). No lymph nod swelling and splenomegaly was found. Her CXR and ECG were both WNL. The urinalysis was WNL, including negative Bence-Jones protein.
The results of her routine laboratory examination showed severe anemia, thrombocytopenia, and markedly decreased cholinesterase (ChE) and total cholesterol (T.Chol) levels. Initially, these findings were considered to be compatible with the pattern of severe liver insufficiency (Table 1). However, her abdominal ultrasonographic examination revealed that she had only mild chronic hepatitis, but not liver cirrhosis.
Furthermore her serologic data also were extraordinal. In which, the IgG and IgA levels were remarkably high (Table 2).
Table 1 (Nov 12 '08)
|
|
T.Bil |
AST |
ALT |
LDH |
ALP |
ChE |
T.Chol |
FBS |
Cr |
Ca |
WBC |
Hb |
MCV |
Platelet |
HBs Ag |
HCV |
|
PATIENT |
1.1 |
51 |
28 |
209 |
192 |
41 |
72 |
88 |
0.46 |
9.4 |
1.9 |
8.3 |
109.1 |
51 |
+ |
- |
|
Standard |
<1.2 |
8-37 |
4-48 |
110-217 |
106-320 |
188-452 |
130-219 |
60-109 |
0.46-0.82* |
8.5-10.5 |
4.0-8.0 |
11.3-14.9* |
79-99 |
120-406 |
|
|
|
|
mg/dL |
IU/L |
IU/L |
IU/L |
IU/L |
U/L |
IU/L |
mg/dL |
mg/dL |
← |
x1,000/μL |
g/dL |
FL |
x1,000/μL |
EIA |
EIA |
* standard: for female
Table 2 (Nov 12 '08)
|
TP |
Alb(n) |
A/G |
ZTT |
TTT |
CRP |
Alb |
α1 |
α2 |
β |
γ |
IgG |
IgA |
IgM* |
IgD |
IgE |
RF |
ANA |
DNA |
SS-A |
SS-B |
|
11.5 |
2.3 |
0.25 |
79.0 |
31.5 |
0.1 |
2.56 |
0.20 |
0.37 |
3.88 |
4.58 |
4854 |
4120 |
66 |
<1.0 |
954 |
6840 |
1280 sp |
4.2 |
+ |
+ |
|
6.5-8.3 |
3.8-5.3 |
1.2-2.3 |
3-12 |
<5 |
0.4 |
|
|
|
|
|
820-1240 |
90-400 |
62-270 |
<15 |
<170 |
<15 |
<80 |
<20 |
<30 |
- or ± |
|
g/dL |
← |
|
U |
U |
mg/dL |
g/dL |
← |
← |
← |
← |
mg/dL |
← |
← |
← |
IU/mL |
U/mL |
X |
IU/mL |
|
|
:* standard: for female, Alb(n): by nephelometry
Figures(Fig) (Nov 12. '08)
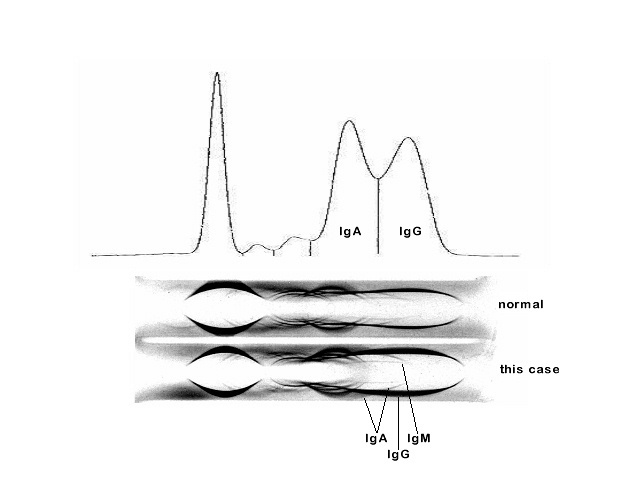
The serum electrophoretic and immunoelectrophoretic patterns are shown in the figures (Fig).
The conspicuous finding of the routine serum electrophoresis (EP=uppermost) was extraordinarily increased beta (β) and gamma (γ) globulin fractions.
It is generally accepted that, as albumin is the representative "monoclonal" protein in EP, only when the figure of any increased globulin peak is as sharp as that of albumin, the peak could be recognized as "monoclonal". Thus, the large and broad beta and gamma globulin peaks of this case were considered to be conposed of only polyclonal immunoglobulins.
The immunoelectrophoresis of the serum (IEP) also showed markedly increased IgA (heavy chain) as the main component of "beta" globulin fraction accompanying much increased IgG as the gamma globulin fraction.
On the other hand, the IEP also showed that the lambda (λ) light chain of this patient markedly increased due to an increase in probable monoclonal component ((lowermost figure).
The coexistence of monoclonal and polyclonal hypergammaglobulinemia in a same patient in a same time, as was seen in this case, is an unusual incident. Especially monoclonal gammopathy usually brings decreases of other immunoglobulin classes. In this patient, the coexistence of gammopathy of two types, poly- and monoclonal, might be occurred as a result of combination of different two disease process developed in an individual, who had had longstanding polyclonal hypergammaglobulinemia recently developed monoclonal gammopathy, or the reverse process (1).
RESULTS OF FURTHER EXAMINATIONS AND COMMENTS
The presence of monoclonal λ light chain suggested that the patient possibly have multiple myeloma (MM). However, by the plane whole body bone radiography, there was no "punched out" lesion, and a bone scintigraphy was negative. Thus, the M-proteinemia, if any, was considered to be the stage of smoldering MM, or monoclonal gammopathy of undetermined significance (MGUS).
Her bone marrow was markedly hypocellular in which M/E ratio was about 5/1. The plasma cell population was not increased. No colony of blastoid cell was found.
Based on the subjective sicca syndrome and the presence of anti-SS-B(La) antibody, a diagnosis of Sjogren syndrome was made, which was accompanying unusual polyclonal gammopathy possibly due to B-cell lymphomas, including mucosa-associated lymphoid tissue (MALT) lymphomas, and complicated by MGUS (2). After admission, daily 20 mg of prednisolone as the agent for therapeutic diagnosis was begun. However, the immunoglobulin levels were only slightly improved within a month, and she discharged with daily 15 mg of prednisolone because she developed steroid-induced psychosis, which was hardly controlled within the hospital. Recently (Jul. '09), as an outpatient, she has been administered daily 15 mg of prednisolone, and her subjective condition was almost well but the unusual hypergammaglobulinemia (over 4,000 mg/dL for IgA and IgG), and slight psychosis were still persisted.
The probable mechanism(s) of the development of serologically detected "liver cirrhosis" is considered as follows: markedly increased immunoglobulin synthesis by plasma cells due to Sjogren syndrome and, if any, accompanying lymphomas competitively consumed amino acids which were usually reserved for protein synthesis by hepatic cells in the liver.
For establishing sharp diagnosis, especially for search the source of the excessive immunoglobulins, further examinations are required. (T.Inoue; Jul 30 2009)
REFERENCES:
1. Wakita M, Kotani T, Murakami M, et al. Tumor-forming IgA (κ-type) multiple myeloma developed into polyclonal hypergammablobulinemia after M-protein loss. Rinsho Ketsueki 1991;32:964-9.
2.. Sakamoto T, Yamashita K, Mizumoto C, et al. MALT lymphoma of the thymus with Sjogren's syndrome: biphasic chages in serological abnormalities over a 4-year period followed thymectomy. Int J Hematol 2009;89:709-13.